What is Prolapse (pelvic organ prolapse?)
The female pelvic organs consist of the uterus, vagina, bladder and bowel. Pelvic organ prolapse can occur when the supporting structure of tissues (muscles, ligaments and fascia) that hold these organs in their correct position become weak or damaged.
Possible causes of this weakening or damage are:
- Pregnancy and childbirth
- Menopause and the aging process
- Excessive pressure on the pelvic floor from conditions such as chronic constipation, chronic coughing, heavy lifting/straining, obesity.
- Diseases that affect a person’s connective tissue.
Pelvic organ prolapse occurs when one or more of the pelvic organs prolapse or bulge into or outside of the vagina.
Common symptoms of prolapse
The signs and symptoms of a prolapse can vary depending on what degree of prolapse you may have, for example some women experience no symptoms while the following symptoms may be experienced with a more significantly prolapsed compartment:
- Feeling of a lump or bulge in the vagina or outside of the vaginal opening
- A heaviness or dragging sensation in the vaginal area or lower back
- Urinary symptoms for example a slow or stop/start urinary stream, urgency or frequency with urinating, a feeling of not fully emptying your bladder or need to go back to the toilet a short time after going, urinary stress incontinence, increased urinating at night.
- Pain or discomfort with sexual intercourse
- Bowel symptoms for example a feeling of incomplete emptying with a bowel action or constipation.
- Recurrent urinary tract infections
Types of Prolapse
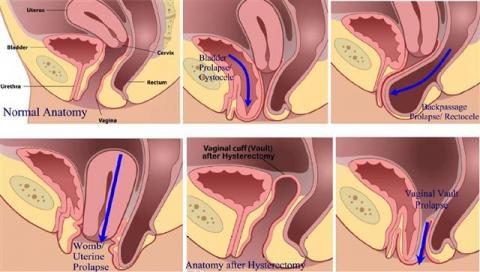
Prolapse may occur in different areas or compartments of the vagina, including the front wall (anterior compartment), back wall (posterior compartment) or the upper part of the vagina/uterus (apical compartment).
Prolapse after hysterectomy
Vaginal vault prolapse – women who have had a hysterectomy can develop prolapse of the vaginal vault whereby the upper portion of the vagina collapses into itself and can fall outside of the vaginal opening.
Diagnosing Prolapse
- History and physical assessment to assess the grade of prolapse
Further assessment may be required including:
- Flexible cystoscopy
- Video Urodynamics
- Abdominal/Pelvic Ultrasound
Treatments provided by our practice
Conservative/Non-surgical treatments for Prolapse
Conservative approaches to manage mild prolapse can include:
- Lifestyle changes - awareness of possible causes of your prolapse and adjusting your lifestyle where required, for example prevent constipation with diet and fluid changes, quit smoking, exercise and weight loss, correct lifting techniques, avoid straining.
- Pessaries – a pessary is a rubber or plastic device that comes in a variety of shapes and sizes, and is designed to fit in your vagina to provide support to the prolapsed organs with the aim of relieving your symptoms. Pessaries must be fitted by a qualified health care provider with expertise in this area and reviewed regularly.
A variety of health care providers can assist you with education and advice on lifestyle changes for your prolapse.
Our practice can assist you with referrals and advice on a conservative approach in the management of all types of prolapse.
Surgical Treatment for Prolapse
The goal of surgery for prolapse is to restore the pelvic organs to their normal position, with a subsequent relief of bladder, bowel and sexual function symptoms.
Cystocele repair is often carried out in conjunction with stress incontinence surgery such as slings. Where a cystocoele occurs a native tissue repair can be performed but for more complex surgery involving multiple vaginal areas or where mesh is warranted we would refer on to one of our collaborative Gynaecological Specialists.
Please note: Dr Jessica Yin is not a Gynaecologist; She is the Consultant Urologist for the Uro-gynaecological Unit at King Edward Memorial Hospital for women and is thus skilled in prolapse assessment and the management of Urogynaecological complications.
Our practice specialises in the care and treatment for patients with prolapse involving the bladder from initial assessment and diagnosis to ongoing care and treatment.
We are able to assess and refer (where required) for prolapse that requires more complex repair or mesh.